US Rep. Kelly leads Tri-Caucus in urging White House, Congressional Leaders on Medicaid priorities
The lawmakers are requesting four Medicaid priorities be included in the next economic reconciliation package.
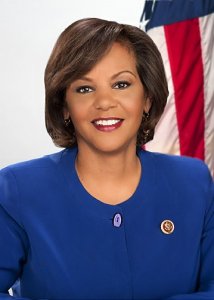
Congresswoman Robin L. Kelly (D-IL) on Monday (April 18, 2022) sent a letter on behalf of the Congressional Tri-Caucus (the Congressional Black Caucus, the Congressional Hispanic Caucus, and the Congressional Asian Pacific American Caucus) urging President Biden and Congressional leaders to include four vital Medicaid provisions in the next economic reconciliation agreement.
The lawmakers are seeking action on providing 12 months of continuous Medicaid and Children’s Health Insurance Program (CHIP) eligibility, 12 months of Medicaid and CHIP postpartum coverage, permanent funding for CHIP and associated policies that facilitate children’s enrollment in coverage; and a solution to permanently close the Medicaid coverage gap in states that have not elected to expand coverage.
“Experts estimate that more than 15 million people could lost Medicaid coverage in the months immediately following the end of the public health emergency. Black and Latino people are disproportionately likely to be enrolled in Medicaid, due in large part to their overrepresentation in low-wage jobs lacking health coverage,” wrote the Members.
“While the share of Asian people enrolled in Medicaid is similar to white people, a number of subgroups make up a disproportionate share of Medicaid enrollees, including Native Hawaiians and Pacific Islanders, Bangladeshi, Burmese, Hmong, Nepalese and Pakistani individuals.”
Together, these crucial policies will help ensure that millions of Americans do not become uninsured when the current public health emergency ends.
The following is the full text of the letter:
The Honorable Joseph R. Biden, Jr.
President of the United States
The White House
1600 Pennsylvania Avenue NW
Washington, DC 20500
The Honorable Kamala Harris
Vice President of the United States
The White House
1600 Pennsylvania Avenue NW
Washington, DC 20500
We, the undersigned leaders of the Congressional Black Caucus, the Congressional Hispanic Caucus, and the Congressional Asian Pacific American Caucus together write to urge you to include four provisions from Build Back Better in the final economic reconciliation legislation to help ensure that millions of Americans do not become uninsured when the public health emergency (PHE) ends. These provisions would require that states provide 12 months of continuous Medicaid and Children’s Health Insurance Program (CHIP) eligibility to children and 12 months of Medicaid and CHIP postpartum coverage; permanently fund CHIP and its associated policies that make it easier for kids to enroll in coverage; and permanently close the Medicaid coverage gap in states that have not elected to expand coverage. Together, these policies would keep millions of Americans insured after the PHE ends.
The continuous coverage provision in the Families First Coronavirus Response Act prohibited states from disenrolling individuals from Medicaid during the PHE; this policy has allowed millions of people to keep their Medicaid coverage and get the health coverage they need throughout the pandemic. However, when the PHE ends, states will have to begin “unwinding” Medicaid continuous coverage and review whether each Medicaid beneficiary remains eligible. This will be a huge challenge for states, and the risk of mass coverage loss is high, particularly for our communities.
Experts estimate that more than 15 million people could lose Medicaid coverage in the months immediately following the end of the PHE. Black and Latino people are disproportionately likely to be enrolled in Medicaid, due in large part to their overrepresentation in low-wage jobs lacking health coverage. Additionally, before the pandemic they were more likely to be caught in the coverage gap, leading them to forgo insurance and incur medical debt or opt to not seek medical care at all. While the share of Asian people enrolled in Medicaid is similar to white people a number of subgroups make up a disproportionate share of Medicaid enrollees, including Native Hawaiians and Pacific Islanders, Bangladeshi, Burmese, Hmong, Nepalese and Pakistani individuals.
People will lose coverage for a range of reasons. Many individuals have moved during the pandemic, so notifications may not reach them. Others may be unable to get help completing paperwork, and understaffed state agencies may not process cases on time. Still others may no longer be eligible and need help transitioning to other coverage.
Requiring states to provide 12 months of continuous eligibility for children and 12 months of postpartum coverage following the end of pregnancy will help keep people covered. Ensuring that all pregnant people enrolled in Medicaid can get a full year of postpartum coverage is an evidence-based strategy to improve maternal and child health and reduce disparities that have driven this country’s maternal health crisis. In 2019, Medicaid paid for more than 42 percent of all births in the United States, 65 percent of births to Black mothers, and more than 59 percent of births to Hispanic mothers.
And research shows Medicaid coverage significantly improves pregnancy-related health outcomes by increasing access to care — particularly during the postpartum period. A state option for 12 months of postpartum coverage was included in the American Rescue Plan and became available this month. So far, about half the states have taken steps to extend postpartum coverage. The provision is especially important for Black mothers who continue to experience the highest rates of maternal mortality, and Latina mothers who are experiencing increasing rates of maternal mortality. Unfortunately, some states have opted to extend postpartum coverage for only a narrow subpopulation of new mothers, such as those who experience substance use disorders. However, we believe that all new mothers should have continuity of coverage, not just discrete populations.
Similarly, prior to the pandemic, continuous coverage was shown to stabilize children’s coverage and avoid the churn—when eligible people lose coverage and have to reapply— that often occurs when people face barriers to maintaining coverage. Continuous eligibility for children has been an option for states since 1997, but only about half the states have implemented that policy. During unwinding after the PHE ends, churn will likely be at an all-time high as Medicaid agencies struggle to keep up with increased workloads. Continuous eligibility for children and extended postpartum coverage would reduce agency workloads and the chance that children and pregnant women could unnecessarily lose Medicaid coverage or experience coverage gaps when transitioning to the marketplace.
Additionally, it is well-past time for us to make CHIP permanent. CHIP provides health insurance to millions of low-income children and utilizes a number of evidence-based strategies to make it easier for kids to enroll. Making CHIP and its associated policies permanent would also ensure that children who need to sign up for coverage can do so quickly with minimal red tape. Recent guidance from the Centers for Medicare & Medicaid Services specifically cites these helpful policies that promote continuity of coverage and reduce churn after the PHE ends. Making these polices a permanent, national standard would ensure a more orderly process during PHE unwinding and help children and postpartum people stay connected to coverage.
Finally, permanently closing the Medicaid coverage gap, which leaves over 2 million people—most of whom are people of color—without access to affordable coverage, would keep large numbers of people from ending up without any pathway to coverage when the PHE ends. This includes large numbers of young adults who have turned 19 and no longer qualify for children’s coverage, pregnant people who have reached the end of their postpartum period, and parents whose income has gone above their states’ very low eligibility thresholds (for example, $320/month for a family of 3 in Texas) but who still live below the poverty line. None of these individuals will be eligible for Medicaid in the 12 states that have refused to expand. Without action to close the coverage gap, to give them a pathway to affordable coverage, they would likely become uninsured.
We urge you to include these four provisions—providing continuous coverage for children; providing 12 months of postpartum coverage; making CHIP and associated policies permanent; and closing the coverage gap –in any final economic reconciliation agreement to expand and protect health care coverage for many of the most vulnerable children, women, and adults in our country.